The coronavirus pandemic turned the world upside down in 2020, and we are still reeling from its effects two years later. Our medical research and health-care systems have been forced to shift, change, adapt and act quickly to address people’s needs and to save lives.
In a message during Inquirer’s Project Rebound April 28 webinar for Health care, Department of Health (DOH) Undersecretary Rosario Vergeire reports that while we are currently seeing an optimistic decline in active COVID-19 cases, and our health-care systems have gone down to a low risk capacity, she also warns that much still needs to be done for us to fully transition to an endemic phase.
Though it may seem like we’re already seeing the light at the end of the tunnel, health experts from both the Philippines and on the global level warn that the battle is far from won.At the core of Usec. Vergeire’s report and recommendations is the importance of vaccinations as the first step to transitioning safely from a pandemic to an endemic, on all levels, from the personal, to family, workplace and community levels.
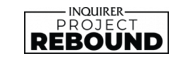
In addition to continued vaccinations, Vergeire also highlights a healthy settings approach to achieve a positive behavioral change that will help in the transition. Healthy settings involve implementing and upholding community standards and systems geared toward better public health. Among examples of the healthy communities standards are ensuring proper ventilation and al fresco seating in restaurants and dine-in establishments, strongly enforcing mask-wearing policies in spaces where there is poor ventilation such as markets and other establishments, opening more public parks and spaces for use, and implementing bike lanes to encourage active transport as well as decongest public transportation.
Acting World Health Organization representative to the Philippines Dr. Rajendra Prasad Yadav further emphasized that the pandemic is far from over, despite what our day-to-day may appear to be. He noted that countries have been testing less and are thus reporting lower numbers.
“We should not be misled by data,” he says. “Yes, the number of cases and deaths are low, and we are moving in the right direction. But if we relax at this stage and say there is no COVID anymore, that may discourage people from using masks, from getting vaccinated and boosted, and that would not be good. We will go back to where we were the past two years.”
Department of Health Undersecretary Maria Rosario Vergeire
How to get to a postpandemic future
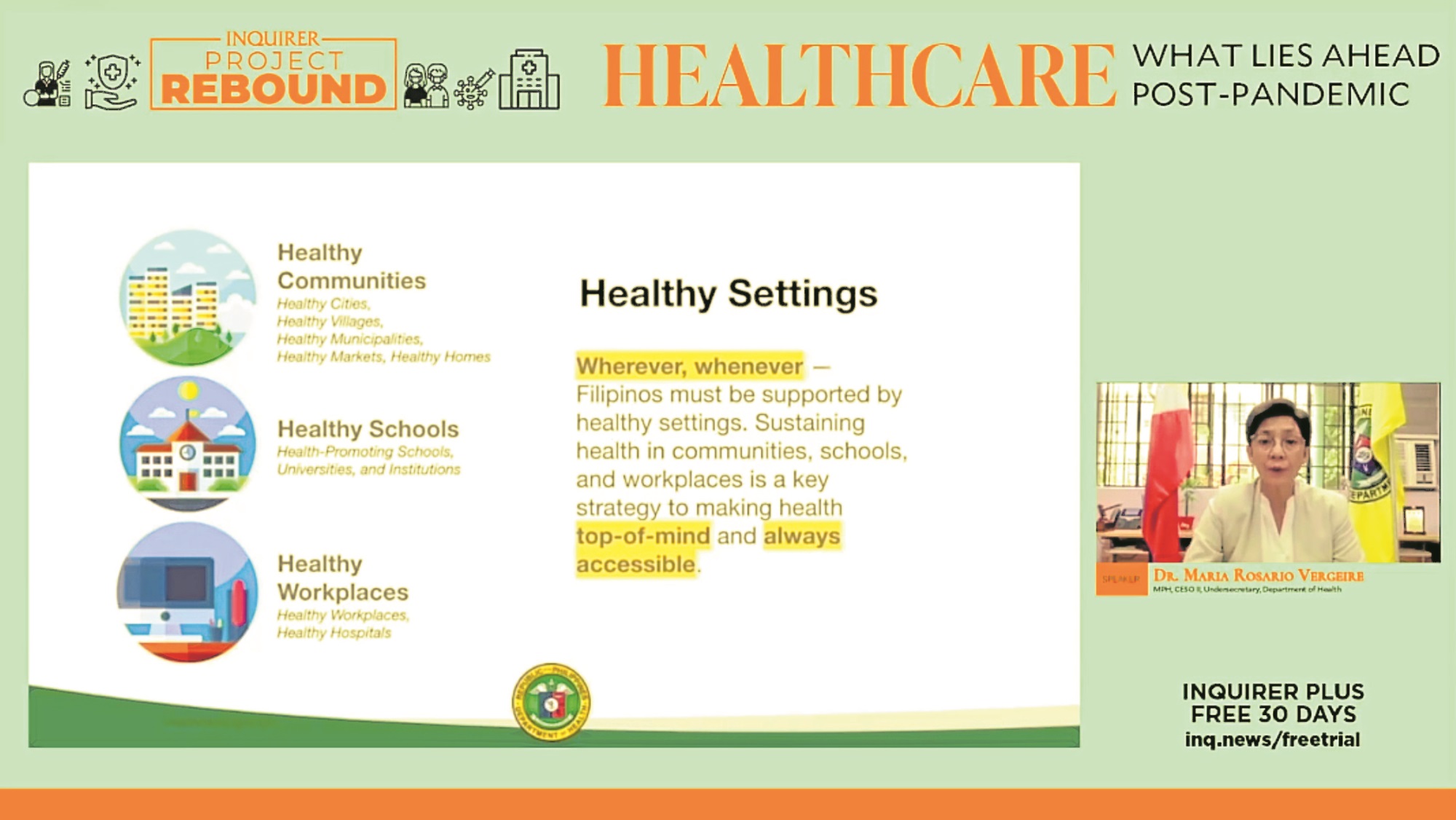
To truly emerge victorious against the COVID-19 pandemic, Yadav shares three main lines of defense. First is the continued use of face masks as personal protection against infections. He lauded the Philippines for being one of the most cooperative countries when it comes to masking, noting that in the country, 90 percent are using face masks.
The next line of defense is to get vaccinated and boosted. The Philippines has not yet reached the ideal level of vaccinations, Yadav shares, which is to have at least 70 percent of each barangay fully inoculated. He says it is imperative to raise the vaccination rate before the country can fully move into a postpandemic phase.
The final line of defense, according to Yadav, is to ensure an adequate supply of oxygen and drugs are available to prevent deaths due to COVID.
“We should not have to reach this if we have proper masking and vaccinations and boosters,” he says, “but if we reach [this point] we must have an adequate supply.”
These three lines of defense are the immediate areas of concern amid this current pandemic. Yadav adds that it is important for countries to rethink priorities, look at the current inequities, and consider who may have been left behind in terms of COVID and development, to ensure that postpandemic will not just be a regression to the old systems.
He also emphasizes rebounding together, through focusing on “self-care”—meaning building a stronger health literacy that would allow people to address simple health concerns on their own, without having to resort to physically visiting health facilities. He also highlights the continued use of “telecare,” and outreach services to reach more people and keep them healthier and more resilient in facing future pandemics.
Lastly, Yadav urges people to care for the environment. The climate crisis coincides and overlaps with the current COVID crisis. “Unless we care for our planet, our health will continue to suffer. Not just from COVID, but from other ailments, too,” Yadav says.
Acting World Health Organization Representative to the Philippines Dr. Rajendra Prasad Yadav
Technology in health care
The pandemic has seen a rise in digitization of many services, health care included. KonsultaMD, the current leading telehealth company in the country, recorded a 2,000 percent growth in consultations in 2021, proving just how essential digital health services have become amid the global COVID crisis.
While the digital health landscape in the Philippines has already been established and has been growing since the late 90s through the National Telehealth Center, much remains to be done for a full and effective adoption of digital health in the country.
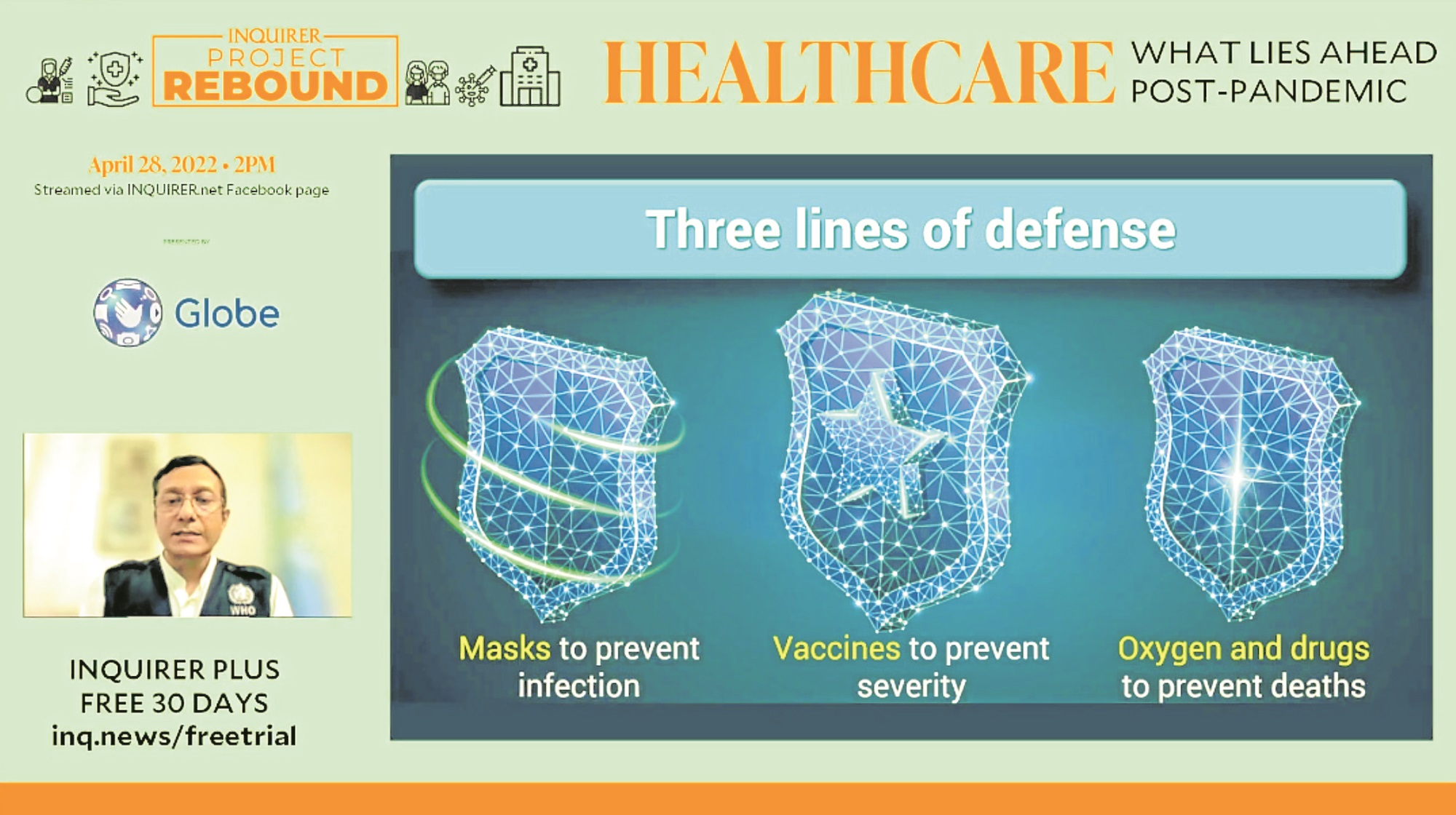
Dr. Michael Caampued, a founding board member and current president of the Philippine Society for Public Health Physicians and partner for the nongovernment organization Alliance for Improving Health Outcomes, goes into detail about the state of digital health in the country, as well as its challenges and potential future.
Advancing technology along with the occurence of the COVID-19 pandemic are among the key factors that contributed to current adoption of digital health in the Philippines.
Caampued notes that in the pandemic alone, telehealth and health apps were on the rise. Digital health solutions such as these have been useful in addressing the need for further outreach. He also notes that this promoted better governance and management of health systems thanks to solutions like health registries, COVID trackers, data dashboards and the vaccine database.
And while the telemedicine field has grown, he also noted that some challenges have mounted. In some areas, he says, there is still a difficulty in transitioning away from analog practices, and there remains a disconnect between public sector ICT (information and communications technology) solutions and patient and provider experience. He attributes this to the existing digital divide, as underdeveloped areas and sectors have inadequate access to digital services and connection, as well as limitations in technical leadership, or tech-abled leaders that can make ICT solutions happen.
Edward Booty, CEO of community health-care social enterprise reach52, echoes the sentiment. He adds, “It’s a luxury of the rich versus a reality of the poor in all markets because still a lot of these digital services [are more accessible for] richer people, not the poorer people.” Hence reach52’s focus on outreach, bringing health care to far off barangays.
Another key challenge Caampued raises is the “asynchronous pace of national and local development.” He says that local governments tend to be faster in making use of digital health solutions, while the wider-scale national level lags behind.
Digital infrastructure is also seen as a barrier to continued success, he notes, as the country currently has a low digital adoption index. There is currently poor access to high quality internet, which also comes at high costs, but with slow download speed.
Despite this, there is still enormous potential for the Philippines in the field of digital health. The country just needs to catch up in terms of infrastructure and inclusivity of access, Caampued says. To achieve this, the whole of government and society must work hand in hand and participate.
The private sector has also been striving to bring telehealth closer and more accessible to patients. KonsultaMD, which reported massive increase in use and consultations over the pandemic, boasts having more than 1,600 doctors on board the platform, which can be accessed by patients of any condition 24/7, without any need for prior appointments.
It has also been noted by the DOH in prior reports that the pandemic has also brought about a mental health crisis. In August 2021, the National Center for Mental Health reported that calls to their crisis hotlines increased fourfold since the pandemic. At the height of the pandemic, students and educators were also found to be the most susceptible to psychological distress. In response, KonsultaMD has also made it possible for those with concerns or questions to consult licensed psychiatrists through the platform.
Dr. Michael Caampued, a founding board member and current president of the Philippine Society for Public Health Physicians and partner for the nongovernment organization Alliance for Improving Health Outcomes
The future of health care
The changes and adjustments brought about by the limitations of the pandemic has opened opportunities and realizations for the health-care industry. Philippine Alliance of Patient Organizations board member Karen Villanueva notes that now we’ve already seen how much more we can transform the health system.
She cites giving people or patients more voice in health policy-making, and prioritizing how to bridge the digital divide so as to reach those with poor access to health care. And since the pandemic has already made digitization of health services more widespread, she encourages more stakeholders in the health system to use the digital tools for the convenience of patients.
At the same time, Villanueva says it is also important to incentivize and build the capacity of health-care providers so that more people can be served and provided care to.
Former Ateneo School of Medicine and Public Health dean Dr. Manuel Dayrit, in closing, emphasized the need to continue improving health governance. Better governance, combined with increased investments in health can ensure better services for Filipinos, he says. But this must first be preceded by good governance.
“Increased investments with poor governance will only result in wasting resources,” he warns.
Talking about what lies ahead of the health-care field postpandemic, Dayrit reiterated the insights also echoed by the panelists. Interventions such as tech innovations and information technology-powered services will ensure that the country can be prepared against future pandemics. This in turn, also covers ensuring that each Filipino will be able to get basic health services they need.
“The Universal Healthcare Law already mandates these priorities. Let’s get these priorities done,” Dayrit says.

Dr. Manuel Dayrit, former Ateneo School of Medicine and Public Health dean